Our lead program is focused on neurotrophic keratitis (NK), a rare ocular surface disease where loss of corneal sensation prevents the eye from detecting injury and initiating repair. By targeting the intracellular barrier that stalls healing, we aim to redefine the treatment landscape for patients with limited options today.
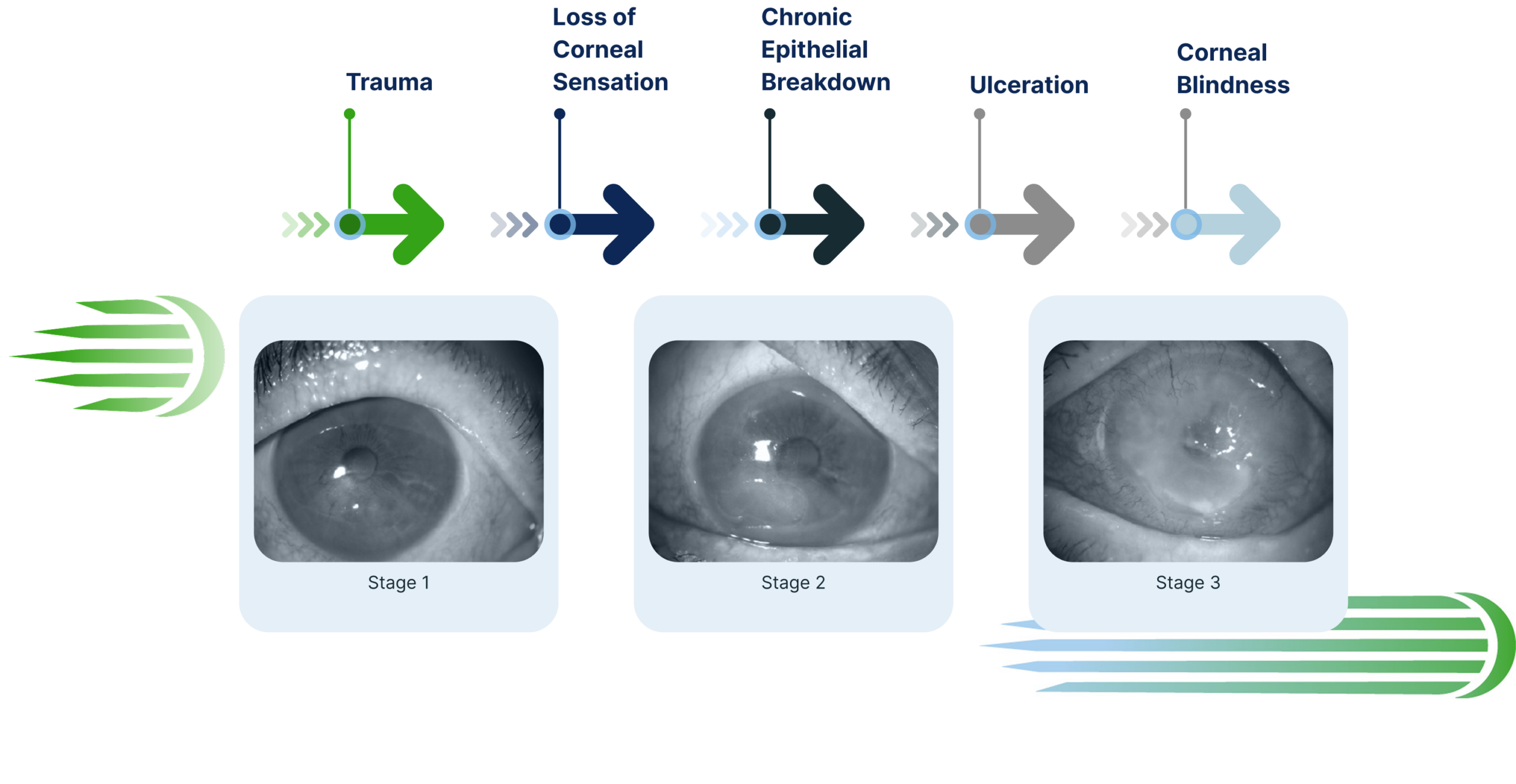
NK is a degenerative ocular surface disease affecting approximately 150,000 people in the U.S., where corneal nerves become damaged and sensation is lost.¹ Without these signals, the eye cannot detect injury or activate the healing processes needed to protect vision.
The result is a progressive condition marked by:
Current therapies focus largely on protection or external stimulation, often with burdensome dosing schedules and variable results. There is a significant need for a treatment that restores the biology of healing itself.
Neurotrophic keratitis represents a clear opportunity to demonstrate the power of pro-regenerative medicine because its underlying biology aligns directly with our intracellular target, FL2. When the cornea loses sensation, the repair process stalls — creating a well-defined need for a therapy that can restore cell movement and support true healing.
The clinical endpoints in NK are clear and measurable, allowing us to translate our preclinical success into meaningful, patient-centered outcomes. By beginning in NK, we can bring real benefit to patients with urgent unmet need while establishing a strong foundation for expanding our platform across other tissues.
Here’s how it works:
Temporarily silences the intracellular enzyme that restricts cell movement and stalls healing.
Restores coordinated epithelial migration and supports corneal nerve regeneration.


Accelerates corneal re-epithelialization for faster early-stage repair

Improves transparency, reducing edema and scarring

Restores nerve architecture, supporting long-term corneal health

Enhances epithelial structure, with more organized cell layers versus controls
Beyond burns, MCR-231’s mechanism suggests possible relevance in other ocular surface injuries and post-surgical healing environments where improved epithelial closure and nerve recovery could significantly benefit patients.
As additional studies progress, we aim to expand the role of pro-regenerative siRNA therapies across a wider range of vision-threatening conditions.